Behavioral Healthcare
-

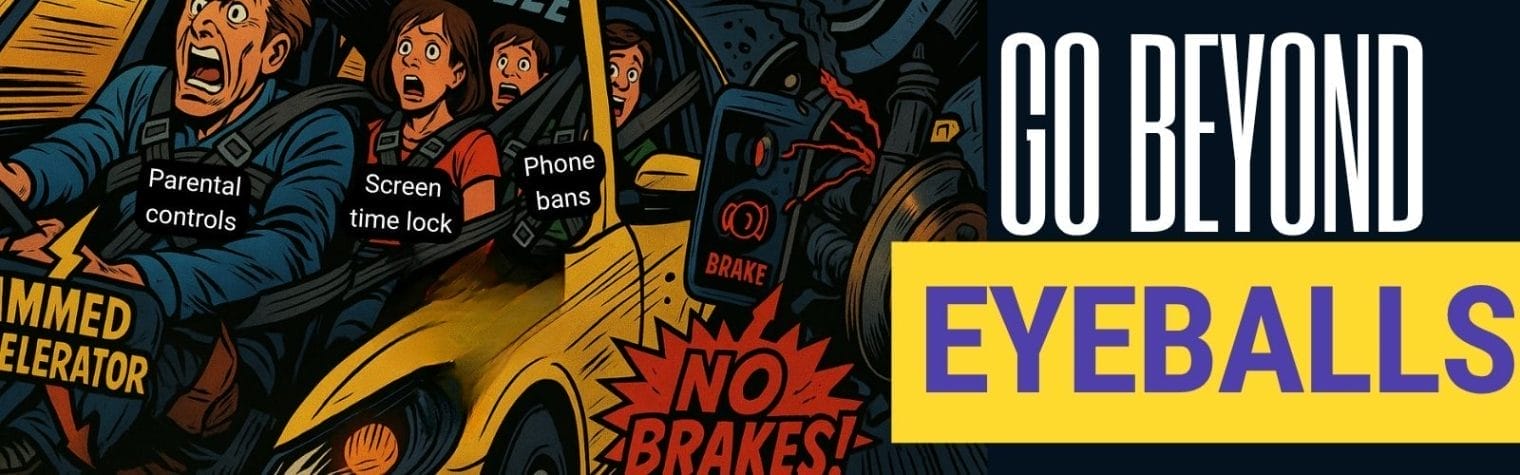
Beyond Eyeballs: Pay for Outcomes, Not Addiction
After several high-stakes responsible-tech applications and helping my daughters through college applications, I finally took a Monday off. Sauna. Cold plunge. Steam. Massage. Except…everywhere the blue light from screens stole the stillness. Signs on the changing room doors banned phones; guests had signed waivers agreeing to it; steam rooms could damage devices. None of it
Read more about Beyond Eyeballs: Pay for Outcomes, Not Addiction
-

From Passive Consumers to Active Shapers: Technology’s Second Chance
We’ve made so much “progress” that we can now order food, learn, and work without ever seeing another person. But is that really true progress or just convenience that erodes our humanity and quality of life? We’ve traded a handful of close friends for thousands of followers—and feel lonelier than ever. We’ve gone from exploring
Read more about From Passive Consumers to Active Shapers: Technology’s Second Chance
-

curaJOY helps adapt behavioral healthcare to different cultures
“The real danger is not that computers will become like humans, but that humans will be treated like computers.” – Sydney Harris OR another one-liner I’d like to state – “The real challenge with AI isn’t making it intelligent, but making it understand people the way we understand each other.” – Geoffrey Hinton (paraphrased) At
Read more about curaJOY helps adapt behavioral healthcare to different cultures
-

When Speed Hurts: Why We Built Our Behavioral Health Solution the Hard Way
Our booth at the AI Show @ GSV + ASU was tiny—just 3×3. We were flanked by past winners of the Tools Competition, NewSchools Venture Fund, and Fast Forward Accelerator—programs we’re now going through ourselves. It was inspiring to be among them—but I’ll admit, I had a moment of doubt. Had I waited too long?
Read more about When Speed Hurts: Why We Built Our Behavioral Health Solution the Hard Way
-

From Big Booths to Bigger Impact: Building AI with Youth
More than 10 years ago, I led teams in 20×30 double-decker booths at major trade shows. CES, NAMM, Infocomm, ProLight+Sound. Big budgets, big lights, big business. This year, I found myself leading 15 first-timers in a 3×3 space. Smaller footprint. Wildly bigger impact. But let me back up. We signed up for the show just
Read more about From Big Booths to Bigger Impact: Building AI with Youth
-

The Link Between Mental & Physical Health and Academic Success
Navigating college life can be challenging, with a constant juggling act between exams, study sessions, and various personal obligations. Amidst this hustle, it’s essential to remember that prioritizing your mental and physical health isn’t just about feeling good—it’s crucial for achieving academic success. Research indicates that when we take care of our body and mind,
Read more about The Link Between Mental & Physical Health and Academic Success
-

Understanding Behavioral Health for Learning
Behavioral health encompasses our emotional, social, and psychological well-being, significantly influencing our thoughts, actions, and interactions. For students, good behavioral health is essential—not just for their happiness but for their ability to learn, achieve academically, manage stress, and build positive relationships. Importance of Behavioral Health for Students Supporting Behavioral Health Students can foster behavioral wellness
Read more about Understanding Behavioral Health for Learning
-

Parenting Is Hard. The Advice Is Confusing. What’s the Real Solution?
Parenting: A Life-Diminishing Factor? I couldn’t believe it when a colleague told me that research suggests parenting is one of the most stressful roles an adult can take on. It made me pause—how could something so deeply meaningful also be so exhausting? But then I looked around: parents today are juggling work, life, guiding kids
Read more about Parenting Is Hard. The Advice Is Confusing. What’s the Real Solution?
-

Leaning In on Nonprofits in Uncertain Times
Sometimes, the world just sucks. Jobs disappear overnight, bills skyrocket, and each day seems to usher in a new crisis. I’ve witnessed firsthand how these harsh realities—the uncertainty of 2025—can knock the wind out of families and erode our sense of hope. But I’m not here to wallow. It’s clear people need help, and our
-

When and Why Are Functional Behavior Assessments Done?
In our last post, we broke down what a Functional Behavior Assessment (FBA) is—a systematic process for identifying the underlying reasons behind challenging behaviors. But when exactly should an FBA be conducted, and why is it so important? When Is an FBA Needed? FBAs are typically conducted when a person’s behavior significantly interferes with their
Read more about When and Why Are Functional Behavior Assessments Done?
-

Unlocking Better Behavioral Support: How AI is Transforming Functional Behavior Assessments
Imagine a child struggling with severe emotional outbursts in school, a teen engaging in self-injurious behaviors, or an adult with autism experiencing daily frustration due to communication barriers. Families and educators often feel overwhelmed and unsure of how to help, leading to trial and error approaches that can frequently cause more harm than good. This
-

Unlocking Functional Behavior Assessments Funding
A mother once told me she felt like she was fighting battles on multiple fronts, barely holding on. Her 11-year-old son, bright and curious, had been labeled ‘disruptive’ at school. He wasn’t misbehaving on purpose—he just couldn’t sit still or follow directions like his classmates. When he pushed or shoved, she had to leave work
Read more about Unlocking Functional Behavior Assessments Funding