There’s an unspoken game all the rage in behavioral healthcare–ghost networks. It is a silent crisis that is largely overlooked but causing real damage to families seeking care. Despite assurances that behavioral healthcare is accessible, these ghost networks make it nearly impossible to get the help we need.
Two years ago, my family was hit hard by a wave of losses—deaths and illnesses of people close to us. To make matters worse, just a week before school started, one of my daughter’s teachers tragically committed suicide. I knew firsthand how difficult it would be to secure an appointment (having been down this road too many times), but given how much we needed grief counseling, I steeled myself for the inevitable wild goose chase. The emotional toll was simply becoming too much.
The Frustration of Ghost Networks
Our pediatrician gave us a list of mental health providers, and I reached out to our insurance company for an appointment. They handed me yet another list of providers. My kids’ school also sent out communication, assuring all parents and students that grief counseling was available. Armed with these resources, I began calling. I contacted 15 different providers and agencies. Out of those, three had automated messages saying they weren’t accepting new clients. I actually spoke to just two, both of whom placed us on a waitlist.
Ghost networks—providers who are either no longer part of the insurance network or may never have existed—are a harsh reality. A Senate Finance Committee investigation found that an astounding 80% of Medicare mental health providers were “ghosts,” unreachable, not in-network, or not taking new patients.
Real-Life Impact on Families
Fast forward to today, and my daughter is still waiting to talk about her dead teacher, along with a lot of other issues that have piled up in the meantime. I’m a parent who deeply values emotional wellness and I’ve made countless calls, and dedicated endless hours to navigating this broken system. The school says there’s grief counseling, but there’s no clear way to schedule an appointment, and no one is available. What happens to children whose parents cannot play this waiting game?
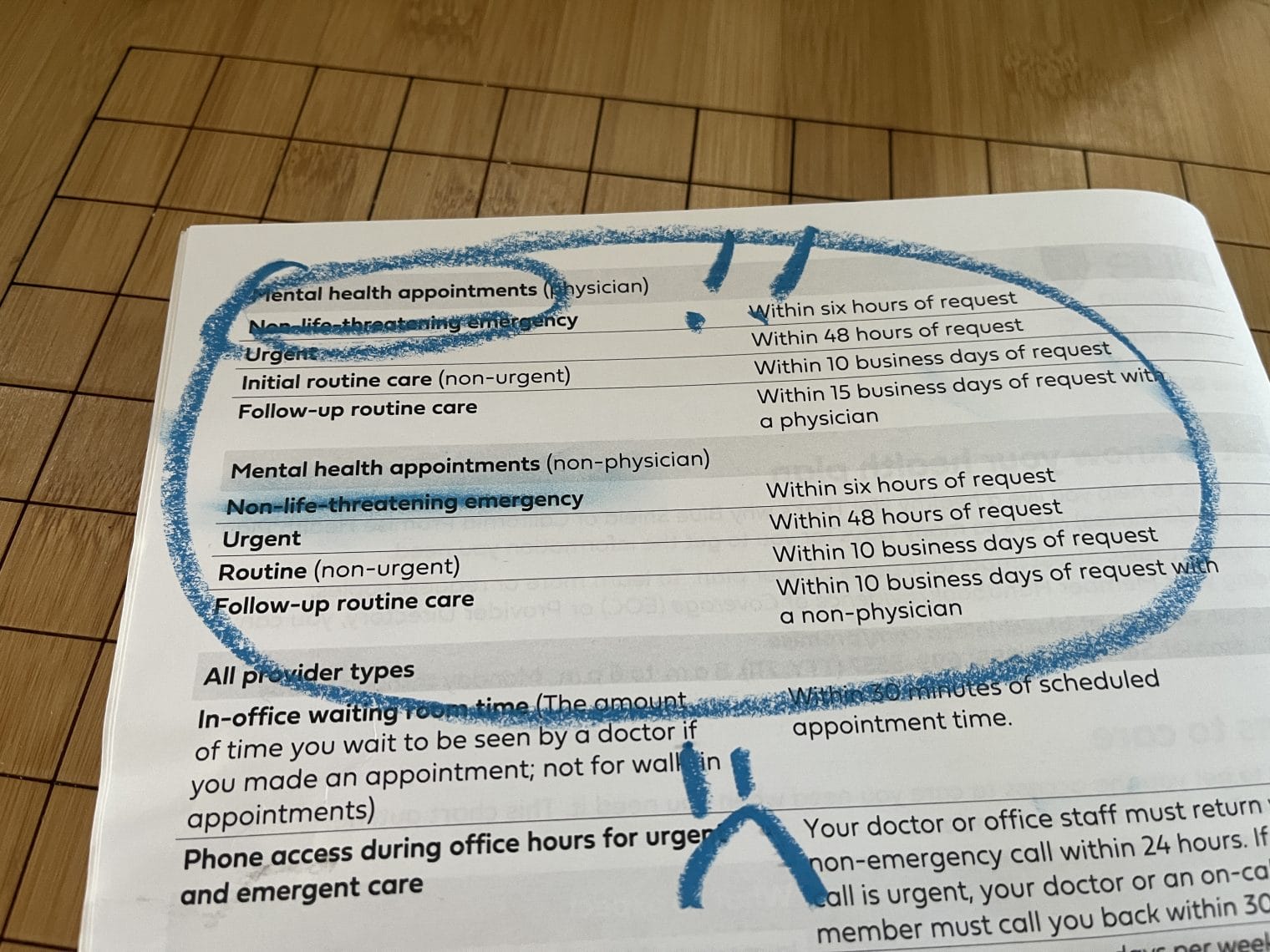
Insurance policies and mental health legislation promise that we are guaranteed a non-emergency behavioral health appointment within two weeks of a request. But who’s holding them accountable? How is this being tracked? I thought about doing an exposé on this impossible journey of getting mental health care for my family. But with children who still need help, I realized I couldn’t afford to make enemies of a system I still depend on.
The Gap Between Mental Health Legislation and Reality
Today, my kids are home sick, and I’ll be speaking with their pediatrician through a video visit in a few hours. (Yes, there is a big difference in getting care for physical illnesses that can quickly accompany prescription scripts.) She may ask me again why I haven’t arranged ongoing weekly therapy for them. After all, she’s made the referral several times. Once again, I’ll be the “good mom” and start calling through every provider on the list. But I already know—it will take hours away from an already overstretched mom, and we’ll likely end up back where we started: waiting.
Ghost networks are not just a glitch in the system—they are the system. The gap between the availability of mental health care and the promises of insurance companies and legislation is a deepening crisis for families across the country.
Maybe I’ll decide to do 100% private pay just so that somebody sees us–I just always naively thought that’s what health insurance was for. No family should have to navigate an endless maze to get the mental health services they desperately need. What’s your experience been?


Leave a Reply